Functional quadriplegia still a documentation, coding headache for most healthcare organizations
By Brian Murphy
Functional quadriplegia (ICD-10-CM code R53.2) was a big deal back in my ACDIS days, for a few reasons:
1). It wasn’t a term physicians typically used/documented, even though it’s a common condition among certain populations. Physicians and other caregivers are more apt to use “bedbound, total care” or other such terms.
2) It’s got payment ramifications. R53.2 is a major complication/comorbidity (MCC). It also has impact in risk adjustment, grouping to CMS-HCC 70 in Version 24 and 180 in V28.
3) Because of 1 and 2, payers deny it—especially if it is the only MCC reported on a claim.
But times have changed. Coding software has improved and the term has perhaps become more commonplace through use and education.
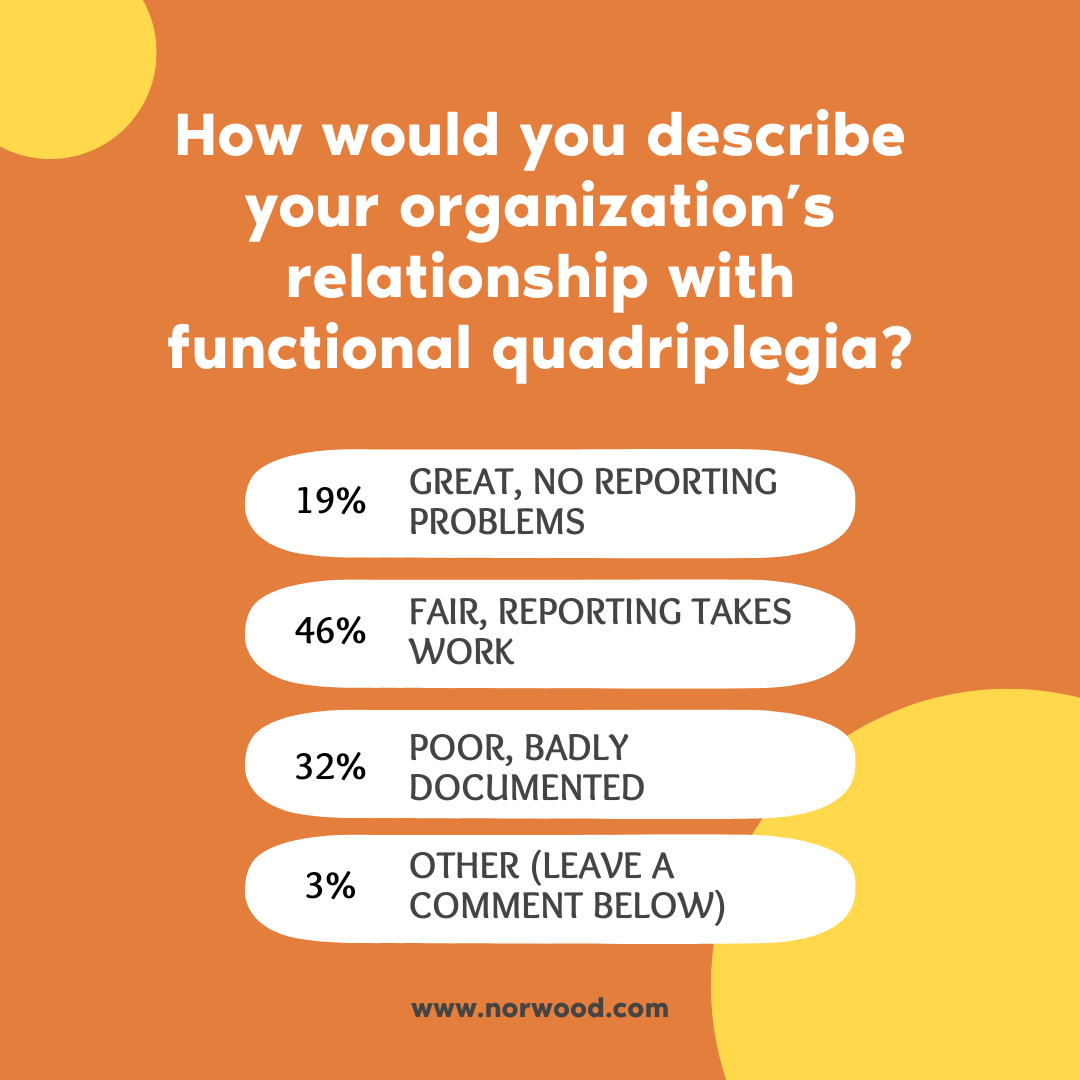
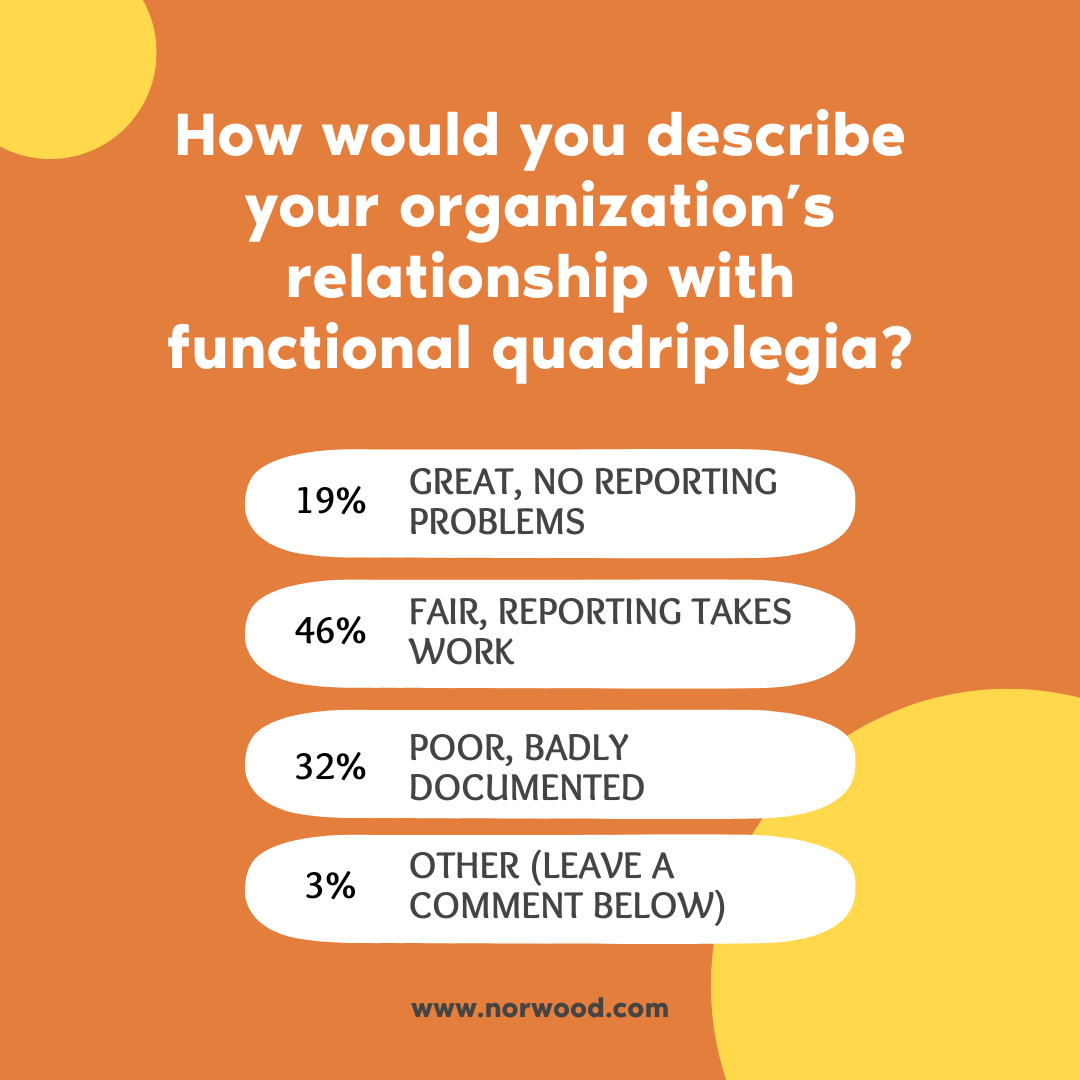
Last month I put up a poll on LinkedIn to see where folks are with compliant capture of this condition. As you can see, results vary. But the largest bucket of respondents (46%) selected “fair, reporting takes work.” Only 19% said they had no reporting problems with this diagnosis.
If you answered fair or poor to the poll, I’ve gathered some helpful resources to help you get on track.
- Functional quadriplegia is defined as complete immobility resulting from severe physical disability or frailty, without physical injury or damage to the brain or spinal cord. It’s important to note that this condition is distinct from neurological quadriplegia, which is due to spinal cord injury and is coded differently. The Pinson and Tang article below delineates this well.
- ACDIS offers the following tips for consideration: “Functional quadriplegia should be considered with patients diagnosed with severe, end-stage dementia or an advanced progressive neurodegenerative disorder such as multiple sclerosis, amyotrophic lateral sclerosis (ALS), cerebral palsy, or Huntington’s disease. The nursing admission functional assessment should provide clinical validation demonstrating the patient’s inability to move extremities, requiring total assist with activities of daily living. These patients often present with contractures and muscular atrophy.” A long-term nursing home patient admitted to an acute care hospital for treatment would be a candidate.
- R53.2 has the following Excludes1 notes, Frailty NOS (R54); hysterical paralysis (F44.4); immobility syndrome (M62.3); neurologic quadriplegia (G82.5-); quadriplegia (G82.50). As a reminder an “Excludes1” note in ICD-10-CM means that these conditions cannot occur together and should not both be reported.
- It’s rare to have R53.2 as a principal diagnosis, so CDI professionals should review the record for the underlying disease process and be prepared to query the provider if absent. ACDIS notes that the reason for an acute care admission for these patients is often a complication resulting from the immobility.
- This condition should not be expected to improve with time or treatment, but it should be captured because the resources expended on these patients are considerable (see ICD-10 Monitor article below).
- Other conditions that may be present with R53.2 include pressure ulcers and malnutrition.
- AHA Coding Clinic, Fourth Quarter 2008, p. 143, contains additional information for compliant reporting. Review that entry with your coding and clinical teams.
References
- ACDIS, 2025 Pocket Guide; “ACDIS tip: Functional quadriplegia”: https://acdis.org/articles/acdis-tip-functional-quadriplegia
- ICD-10 Monitor, “Functional Quadriplegia: A Code for a Real Condition”: https://icd10monitor.medlearn.com/functional-quadriplegia-a-code-for-a-real-condition/
- Pinson and Tang, “Functional Quadriplegia: Not Due to Spinal Cord Injury”: https://www.pinsonandtang.com/resources/functional-quadriplegia-not-due-to-spinal-cord-injury/
Related News & Insights
Top 10 Best Practices for Compliant Use of Point of Care Technology
By Jason Jobes, SVP Solutions Technology is a must for ensuring complete and accurate depiction of patient…
Transcription to Trailblazer: Glenda Bocskovits’ outpatient CDI journey
Listen to the episode here. Outpatient CDI is not a traditional discipline—and so it stands to…


